By Linda J. DiPersio, MSM, MSHC
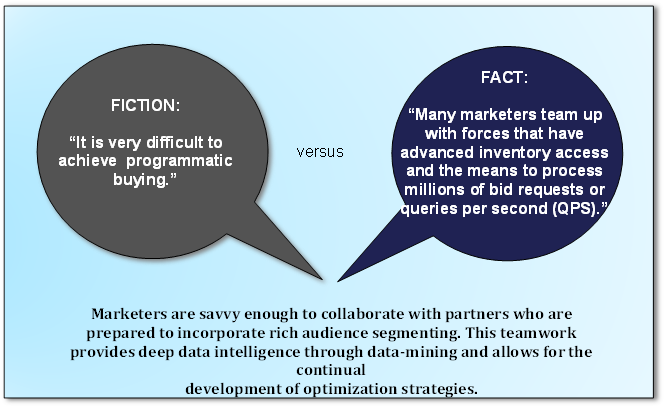
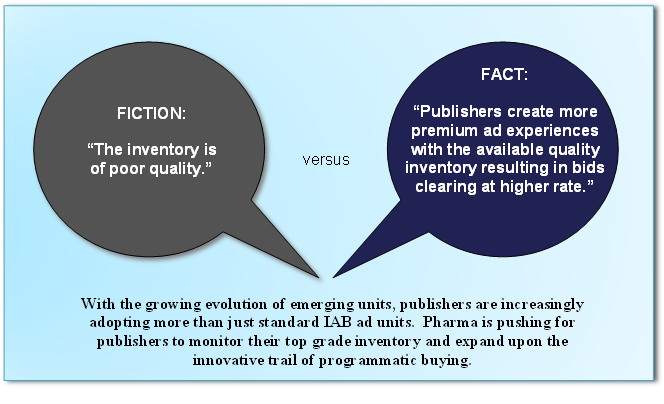
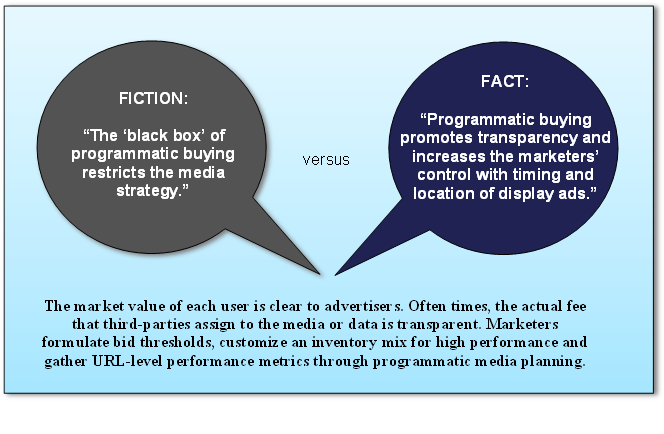
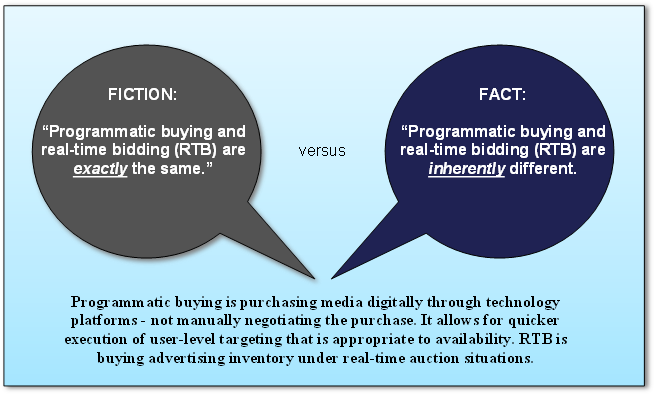
A recent eMarketer study projects that by the end of this year 63% of the overall digital display ad spending in the United States will be attributed to programmatic media buying – and this figure is estimated to soar towards 83% in 2017. In the pharmaceutical industry, programmatic buying uses software interfaces and algorithms to define and analyze specific traits of patients who have a strong inclination to purchase certain medications over others. This data allows digital ad spaces to be tailored to patients more accurately, which influences and supports a patient-centric media strategy in a positive way. The skillful use of programmatic buying within this platform not only depends on educating marketers to recognize the myths but also on encouraging them to follow the trends that will lead to an increased level of patient centricity and greater financial success and efficiency.
Fictional vs. Factual Information about Programmatic Media Buying

2016 Trends in Programmatic Buying
Engaging Purchase-Based Targeting (PBT). With (PBT), marketers analyze segments of small groups of individuals that bought the product previously and then conduct exact image modeling to increase profits by finding more patients who are willing to buy. Behavioral and contextual data attributes enhance this digital segmentation.
Planning with Direct Automation. Advertisers create audiences inside their Data Management Platforms (DMPs) with automated guaranteed procurement. They push them directly to a publisher’s ad server that participates in user-matching.
 Managing Global Frequency. Marketers effectively map users to all of their devices, match users across a myriad of platforms and determine frequency to an individual. They control their messaging and influence their bidding strategies to usher users into frequency where conversions emerge.
Managing Global Frequency. Marketers effectively map users to all of their devices, match users across a myriad of platforms and determine frequency to an individual. They control their messaging and influence their bidding strategies to usher users into frequency where conversions emerge.
Bringing Talent In-House. Hiring former agencies and vendors, certifying their own technologies and retaining their own data are only a few of the ways that big marketers are consolidating talent internally. They desire an intense and direct connection to experts who specialize in programmatic buying and analysts who are focused on data science.
Closing the Loop with Data. The marketing attribution adage of “50% of my marketing works, but I just don’t know which 50%” is now showing 100% closure with organized substantiation. One example is specific beacon technology that allows marketers to actualize results with a three step process: 1) patients are alerted through social media on their mobile devices about a discount offer through social media; 2) their arrival at the pharmacy is verified and 3) data is integrated with the point-of-sale (POS) system that immediately indicates if the product was purchased.
Permitting Technology to Make Determinations. From the outset, data machine algorithms determine the exact make up and segmentation of the patient giving marketers an advanced and full understanding of the shared features of data attributes. Smoother media planning arises from automatic segment generation.
In conclusion, by understanding fact versus fiction and paying close attention to this year’s trends in programmatic buying, marketers can achieve more effective campaigns on a smaller budget and in a timely fashion. Algorithmic data analysis combined with a transparent, unbiased framework strengthens this type of buying and creates a win-win situation for the patient-centric media strategy. With programmatic buying projections, the pharmaceutical industry currently has the fortuitous chance to track the patient journey with available data delivering deeper, clearer and more concise content in the right place to the right people at the right time.
References:
Kleveno, K. “Debunking 5 Myths of Programmatic Buying.” 360i Digital Agency. (2013)
Loechner, J. “Marketers Face More Pressures Than Just Marketing.” MediaPost (2014)
O’Hara, C. “Trends in Programmatic Buying.” Media Measurement. (2015)
“Mobile Marketers Think Programmatic Advertising Is the Future So Why Aren’t They Using It?” CallFire (2015)
“A Look Inside Programmatic Pricing.” AdWeek (2015).





 In the book “The Innovator’s Prescription: A Disruptive Solution for Health Care,” Clay Christensen, who developed the theory of disruptive innovation, stated, “There are more than 9,000 billing codes for individual procedures and units of care. But there is not a single billing code… for helping patients stay well.” In the pharmaceutical industry, disruptive innovation improves health by generating ideas that create new drugs at the expense of existing ones. It is an alliance between technological advances and new business models that dramatically changes the performance of the industry. The progressive spectrum of disruptive innovation challenges include lessons from the past showing resistance to change, implications surfacing in the present which emerge from cautious analytics and trailblazing dynamics in the future aligned with patient centricity.
In the book “The Innovator’s Prescription: A Disruptive Solution for Health Care,” Clay Christensen, who developed the theory of disruptive innovation, stated, “There are more than 9,000 billing codes for individual procedures and units of care. But there is not a single billing code… for helping patients stay well.” In the pharmaceutical industry, disruptive innovation improves health by generating ideas that create new drugs at the expense of existing ones. It is an alliance between technological advances and new business models that dramatically changes the performance of the industry. The progressive spectrum of disruptive innovation challenges include lessons from the past showing resistance to change, implications surfacing in the present which emerge from cautious analytics and trailblazing dynamics in the future aligned with patient centricity. As the above example shows, the advancement of pharmaceutical innovation efforts are most often prevented by established world views, opinions, customs, attitudes, societal values and complex psychological and emotional issues ingrained in the network of relationships that define individuals singly or collectively. In certain situations, innovation challenges are rejected directly because they are seen as threats to the means of support and character of many stakeholders, such as pharmaceutical companies, Federal regulatory institutions and the American Medical Association, that deploy an intangible but forceful influence on decision-making. Resistance to change in pharma emanates from industry incumbents whose jobs rely on sustaining the existing business model and political power. As Upton Sinclair said, “Never expect someone to understand change when their livelihood depends on not understanding it.”
As the above example shows, the advancement of pharmaceutical innovation efforts are most often prevented by established world views, opinions, customs, attitudes, societal values and complex psychological and emotional issues ingrained in the network of relationships that define individuals singly or collectively. In certain situations, innovation challenges are rejected directly because they are seen as threats to the means of support and character of many stakeholders, such as pharmaceutical companies, Federal regulatory institutions and the American Medical Association, that deploy an intangible but forceful influence on decision-making. Resistance to change in pharma emanates from industry incumbents whose jobs rely on sustaining the existing business model and political power. As Upton Sinclair said, “Never expect someone to understand change when their livelihood depends on not understanding it.” In the future, the drug lifecycle needs to incorporate many facets of patient centricity, including the use of new technologies such as gene- and proteomics, gene therapy, nanotechnology, and Big Data driven predictive analytics. Precision medicine will identify exact patient needs and tailor molecular profiles to create the most beneficial treatment plans for patients on an individual level. New social media tools will allow patients to share information and participate in collaborative discussions with regulators and pharma.
In the future, the drug lifecycle needs to incorporate many facets of patient centricity, including the use of new technologies such as gene- and proteomics, gene therapy, nanotechnology, and Big Data driven predictive analytics. Precision medicine will identify exact patient needs and tailor molecular profiles to create the most beneficial treatment plans for patients on an individual level. New social media tools will allow patients to share information and participate in collaborative discussions with regulators and pharma.

 mproving core competencies, emphasizing cost control, focusing on comparative effectiveness, and elevating market access are part of a new strategic planning process. Payers, such as private insurance plans, pharmacy benefits managers, governments, and employers, have moved to the forefront of the pharma industry. They now strongly desire information about drug safety and efficacy to compare drug cost effectiveness to alternative treatments. In the past, determining how much payers would pay for drugs was a major challenge for marketers. However, most recently economically justifying and identifying the intrinsic value of a certain drug is a more important challenge.
mproving core competencies, emphasizing cost control, focusing on comparative effectiveness, and elevating market access are part of a new strategic planning process. Payers, such as private insurance plans, pharmacy benefits managers, governments, and employers, have moved to the forefront of the pharma industry. They now strongly desire information about drug safety and efficacy to compare drug cost effectiveness to alternative treatments. In the past, determining how much payers would pay for drugs was a major challenge for marketers. However, most recently economically justifying and identifying the intrinsic value of a certain drug is a more important challenge. Creative ways are now engaged to capture treatment benefit through subjective research. These practices demonstrate full product value to patients, regulators, and payers. Patients visually express disease experience with mood boards using a collage of images and/or text that represents their emotions and thoughts with drawings or online platforms such as Pinterest. People receiving medical care also utilize body mapping to indicate the location on their body where they experience signs of disease and pain. Patients tell their story in video diaries, often times using smart phones to point out their disease experience in real time. In prior years, face-to-face interviews and focus groups were sufficient, and drug developers relied on merely clinical outcomes. Nevertheless, currently patients recognize the significance of comprehending and collecting subjective research about patient attitudes, preferences, and experiences.
Creative ways are now engaged to capture treatment benefit through subjective research. These practices demonstrate full product value to patients, regulators, and payers. Patients visually express disease experience with mood boards using a collage of images and/or text that represents their emotions and thoughts with drawings or online platforms such as Pinterest. People receiving medical care also utilize body mapping to indicate the location on their body where they experience signs of disease and pain. Patients tell their story in video diaries, often times using smart phones to point out their disease experience in real time. In prior years, face-to-face interviews and focus groups were sufficient, and drug developers relied on merely clinical outcomes. Nevertheless, currently patients recognize the significance of comprehending and collecting subjective research about patient attitudes, preferences, and experiences. Six Sigma and Lean Manufacturing allow pharma to predict and eradicate errors which boost operational efficiency and increase the chance of quality products and compliance, as opposed to relying on end-process testing. These techniques also optimize resources, control inventory, reduce waste and errors, improve customer service and change the market entirely. They identify and remove the causes of defects while minimizing variability in manufacturing and business methods. These tools employ empirical, statistical methods so that a certain group of people materialize as experts in these methods and become an integral part of the infrastructure of the organization. Presently, profits are declining due to greater competition emanating from generic brands and an increase in errors within the manufacturing process. On the other hand, Six Sigma and Lean Manufacturing offer the possibility of saving pharma an estimated $90 billion dollars internationally.
Six Sigma and Lean Manufacturing allow pharma to predict and eradicate errors which boost operational efficiency and increase the chance of quality products and compliance, as opposed to relying on end-process testing. These techniques also optimize resources, control inventory, reduce waste and errors, improve customer service and change the market entirely. They identify and remove the causes of defects while minimizing variability in manufacturing and business methods. These tools employ empirical, statistical methods so that a certain group of people materialize as experts in these methods and become an integral part of the infrastructure of the organization. Presently, profits are declining due to greater competition emanating from generic brands and an increase in errors within the manufacturing process. On the other hand, Six Sigma and Lean Manufacturing offer the possibility of saving pharma an estimated $90 billion dollars internationally. The National Research Council describes Precision Medicine (PM) as adapting medical treatment to the specific characteristics of each patient. It arranges individuals into subpopulations that differ in their likelihood to contract any particular disease. PM is the advanced and detailed understanding of the root causes of a disease and how best to respond with proper treatment taking into consideration genetic changes and ultimate cures.
The National Research Council describes Precision Medicine (PM) as adapting medical treatment to the specific characteristics of each patient. It arranges individuals into subpopulations that differ in their likelihood to contract any particular disease. PM is the advanced and detailed understanding of the root causes of a disease and how best to respond with proper treatment taking into consideration genetic changes and ultimate cures. Preventive and therapeutic interventions, such as physicians dispensing prescription medications during medical visits, benefit patients without high cost or side effects. Health care professionals have the ability to prescribe the right drug for the right patient at the right time at the right place. Patient savings are realized in terms of time, energy, convenience, and money. Also, better health outcomes are achieved with patient adherence because the early stage obstacle of compliance is removed – the patient taking the time to process the prescription through mail order or at a pharmacy. Furthermore, assigning clinicians the power of POC prescribing confronts the dilemma of health disparities.
Preventive and therapeutic interventions, such as physicians dispensing prescription medications during medical visits, benefit patients without high cost or side effects. Health care professionals have the ability to prescribe the right drug for the right patient at the right time at the right place. Patient savings are realized in terms of time, energy, convenience, and money. Also, better health outcomes are achieved with patient adherence because the early stage obstacle of compliance is removed – the patient taking the time to process the prescription through mail order or at a pharmacy. Furthermore, assigning clinicians the power of POC prescribing confronts the dilemma of health disparities. Relative advantage. Gather an understanding of the ROI and cost mindset of the patient, medical staff, and decision makers.
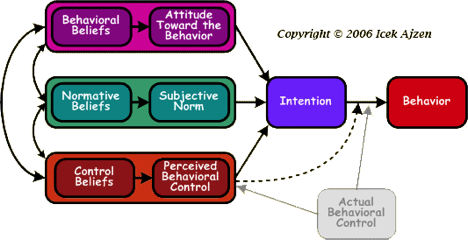
Relative advantage. Gather an understanding of the ROI and cost mindset of the patient, medical staff, and decision makers.



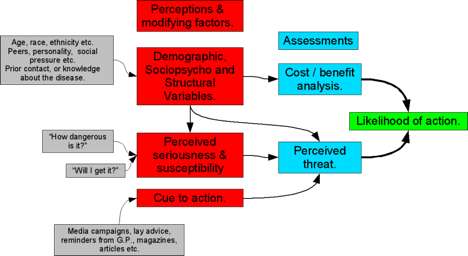
 Health beliefs are predisposing characteristics that are not easily changed.
Health beliefs are predisposing characteristics that are not easily changed. Developing Specific Targeted Strategies
Developing Specific Targeted Strategies Narrow Impact: Fee-for-Value
Narrow Impact: Fee-for-Value Broad Impact: Patient & Lifestyle Autonomy
Broad Impact: Patient & Lifestyle Autonomy