The pharmaceutical industry is one of the most powerful sectors in the United States. The United States government has long realized how much of an influence the industry has had since its origin over a century ago and has regulated the industry as such.
The pharmaceutical industry is one of the most powerful sectors in the United States. The United States government has long realized how much of an influence the industry has had since its origin over a century ago and has regulated the industry as such.
Pharmaceutical companies' largest expenses are research and development costs, which typically range from tens of millions of dollars to several hundred million dollars. With such substantial costs, companies have dedicated more time and energy into developing creative marketing strategies to attract additional consumers.
Here are some of the best marketing strategies that the pharmaceutical industry has seen thus far.
Lobbying and TV Advertisements
Did you know that the United States and New Zealand are the only two countries to allow pharmaceutical companies to advertise their drugs directly to consumers? In the United States alone, pharmaceutical companies have spent countless billions of dollars in order to maintain the ability to advertise directly to consumers over the years. Although lobbying costs are not technically considered marketing expenses, they have a significant effect on direct-to-consumer advertising and, therefore, correspond with advertising expenses.
Although direct-to-consumer advertising in the pharmaceutical industry has several benefits for consumers, it is important that these ads instruct consumers to see physicians prior to deciding on their own that they need to take drugs that are advertised directly to the public. In order to prevent any complications with the medication and to build reliability between consumers and the company, direct-to-consumer advertisements should always encourage consumers to check with their doctor before taking a new medication as well as accurately describe the drug and its purpose.
In 2017 alone, the pharmaceutical industry spent over $6 billion on advertising in direct-to-consumer fashion in the United States. Without lobbying, the government would likely have shut down this form of advertising in the pharmaceutical industry. The industry’s unique ability to keep the direct-to-consumer channel open, along with persistent and coordinated lobbying efforts, make DTC advertising one of the most powerful marketing strategies in the industry.
Drug Discount Cards
Few places outside of the pharmaceutical industry offer coupons that reduce the cost of goods purchased by up to ninety percent. One of the most popular marketing strategies in the industry is the use of drug discount cards. Drug manufacturers work with pharmacies to provide consumers substantial discounts. In return, manufacturers give pharmacies a portion of the original purchase price in exchange for accepting less money directly from consumers.
Pharmacies support discount cards because they encourage people to spend more money on non-drug items inside their stores. In addition, pharmacies that do not accept discount cards have been known to consistently miss out on business in their local markets because the cards have been so widely adopted. Discount cards are both useful and convenient and have therefore been a largely successful marketing tool for the pharmaceutical industry.
Content Marketing
Content marketing is a relatively new form of marketing that has taken the world of business, not just the pharmaceutical industry, by storm over the past few years.
Rather than paying for advertisements that blatantly push messages such as “Buy me now,” content marketing involves authoring helpful guides and blog posts that help consumers learn new information or otherwise offer them something that is completely free of charge.
Content marketing is especially important in pharmaceuticals because it helps build customer loyalty. Most people look up information related to pharmaceuticals when they are concerned about themselves or loved ones due to an illness or medical condition. Accurate and informative guides help build a sense of trustworthiness between the consumer and the company. Connecting with consumers at such significant and emotional times is a solid way of building loyalty to the pharmaceutical company.


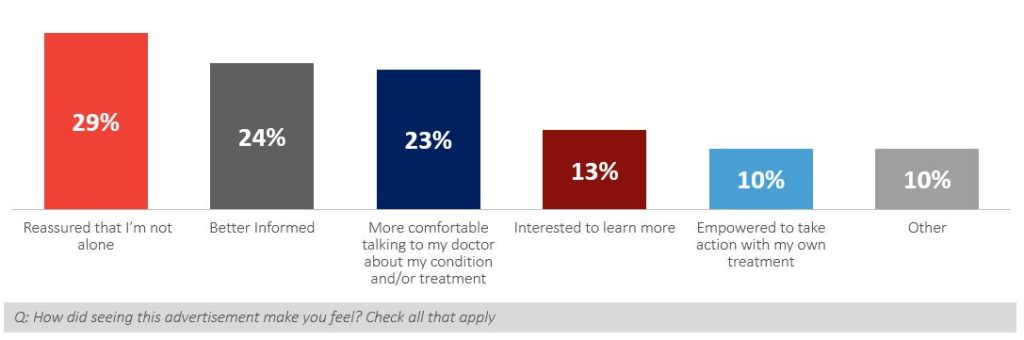
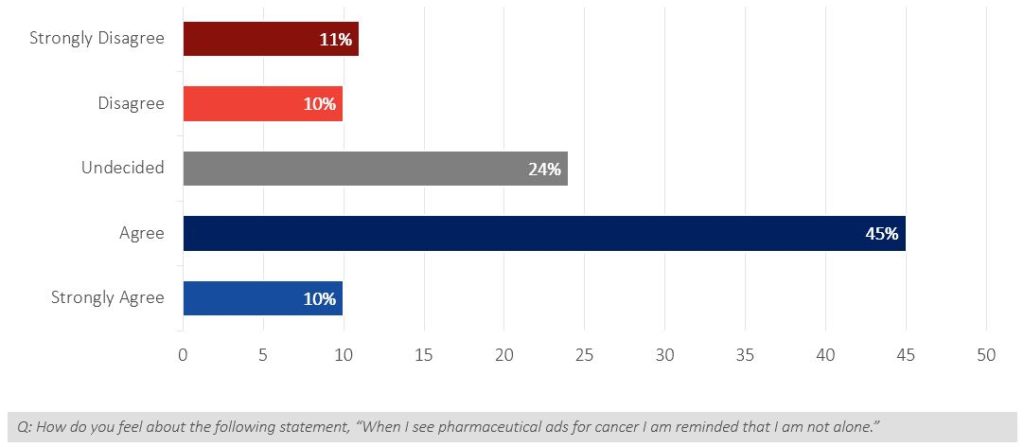
 The results demonstrate that patient engagement solutions at the point-of-care can provide pharma with an opportunity to drive better physician-patient discussions, insert their brand into those discussions and ultimately help educate on better treatment decisions. This is an unprecedented and unique ability to impact both audiences at that magic moment when treatment decisions are being made.
The results demonstrate that patient engagement solutions at the point-of-care can provide pharma with an opportunity to drive better physician-patient discussions, insert their brand into those discussions and ultimately help educate on better treatment decisions. This is an unprecedented and unique ability to impact both audiences at that magic moment when treatment decisions are being made.
 The promotion of products with branding, growth of empathy awareness through an imaginative experience, education, and training are all marketing opportunities that engage patients and doctors while increasing sales, drug compliance, and the number of new drug users. VR produces branding by supporting products that stimulate creativity and evoke senses which results in a unique, complete experience rather than merely a visual presentation. Empathy is built when doctors reaffirm to themselves that they chose their medical careers so they could positively influence humanity. VR serves as training and education for doctors with the optimistic outlook that any mistakes would occur during these simulated patient encounters and not in the real world. By presenting in videos the negative impacts on the quality of life with drug non-compliance, doctors are encouraged to prescribe certain therapeutic medications to keep patients on drug therapy for a longer period of time. This not only equates to improved health, but also an increase in sales and market penetration during growth and maturity drug cycles.
The promotion of products with branding, growth of empathy awareness through an imaginative experience, education, and training are all marketing opportunities that engage patients and doctors while increasing sales, drug compliance, and the number of new drug users. VR produces branding by supporting products that stimulate creativity and evoke senses which results in a unique, complete experience rather than merely a visual presentation. Empathy is built when doctors reaffirm to themselves that they chose their medical careers so they could positively influence humanity. VR serves as training and education for doctors with the optimistic outlook that any mistakes would occur during these simulated patient encounters and not in the real world. By presenting in videos the negative impacts on the quality of life with drug non-compliance, doctors are encouraged to prescribe certain therapeutic medications to keep patients on drug therapy for a longer period of time. This not only equates to improved health, but also an increase in sales and market penetration during growth and maturity drug cycles. Technology Media vs. Traditional Media
Technology Media vs. Traditional Media The theme of this month’s newsletter is consumer trends. Here’s a recent one worth talking about: According to
The theme of this month’s newsletter is consumer trends. Here’s a recent one worth talking about: According to