A Santiago Solutions Group (SSG) in-depth analysis of the most recent enrollment data into ACA exchanges from 38 reporting states revealed that multicultural segments continue to lag way behind the enrollment rate of White Non-Hispanic segment. Less than 100 days away from the third Open Enrollment period, the trends are concerning because so much additional effort was put behind Hispanic, African American and Millennial efforts this past period and the results are marginal at best.
The 38 states in the analysis represent 80% of the country’s population and many of the largest multicultural states in the country such as Arizona, California, Florida, Georgia, Illinois, Nevada, New Jersey, North Carolina, Pennsylvania, Texas, and Virginia were among the 38 states which have broken down the ethnicity of those newly enrolled and renewed in exchange Qualified Health Plans. Included amongst these are all of the Federally-facilitated marketplaces and state-partnership and most of the state-based marketplaces, with notable exceptions like New York, Connecticut, and District of Columbia.
On the surface, the multicultural enrollment rate seems adequate at a 91 index, only 9% below its fair share when considering that 39% of those enrolled at the end of Open Enrollment 2 were from multicultural segments compared to 43% of those eligible in these states. In comparison, 61% of those enrolled have been White Non-Hispanics while 57% of those eligible were of that race, for an index of 108, meaning it is 8% above its fair proportion of eligibles – the segment is enrolling exceedingly well.
Nevertheless, a deeper analysis into each race reveals a much more concerning reality. Hispanics are trailing much further behind than any other group despite all the additional resources that went specifically behind that group in the last open enrollment. While Hispanics make about 15% of those enrolled, they are about a quarter of those eligible, net of undocumented in FPL 139-400 – an index of only 63, that is equivalent to 37% below where the segment should be given its proportion of exchange eligibles. Similarly, the African American segment shows an index of 84, or 16 below where it should be. It is the Asian/Other segment that skews the Multicultural trends with an index of 241, or 141% above where it should be, given that it only represents 5% of eligibles versus 11% of those enrolled so far.
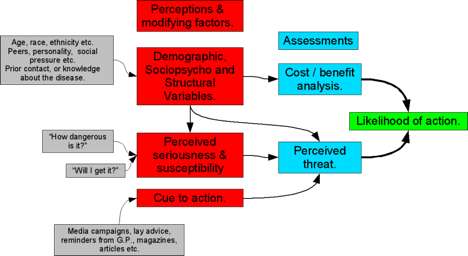
On the eve of the third open enrollment period, the national trends clearly suggest that there are major barriers still standing in front of Hispanic and African American eligibles. There are five major factors at play:
- Lack of Trust in the Government – Mixed status families don’t want to risk exposing immigration status of certain members to official entities and prefer to remain without insurance.
- Poor Value – Deductibles for current plans under the affordable care are far from affordable for many. The plans are still above what many middle-income families can afford relative to their income and other living expenses. Many of them choose to continue to pay-as-they go using urgent care/community clinics and gladly pay the tax penalty. Cheaper plans are critical.
- Ineffective Messaging – On one hand, the plans’ mass media messaging is overly-promising and, on the other hand, the fine print is overly-complex to clearly evaluate. As a result, negative word-of-mouth prevails and a huge portion of the segments are not even seeking official information in-person or digitally.
- Poor Culture & Language Relevancy – While the messages have improved, they are mostly translations or adaptations of communications intended for audiences with high levels of health care and health literacy. For the most part, Hispanic nuances addressing specific barriers and the most effective triggers to adoption have not been brought to the forefront. Exchange communications from the government and insurers are still in cultural diapers.
- Lackluster Customer Experience – The customer experience of those newly enrolled is rampant with stories of poor on-boarding, repeated incorrect bills, systems that don’t reflect conversations with customer service, physicians not in the promised network, communications that are very difficult to understand, inconsistency of in-language communications, and very mixed experiences with call-centers. These unsatisfactory experiences are drowning the exceedingly good ones in physical and digital circles of influence, keeping the undecided eligibles at bay.
At the end of the day, half of the remaining exchange eligibles in these states are Multicultural and 1 in 3 of the overall remaining eligibles (net of undocumented) are Hispanic. The source of growth for ACA is adding critical pressure to getting multicultural engagement, acquisitions, and retention properly focused on the needs of this vast potential. The time for blanket strategies versus dedicated segmentation has passed us. Health insurers which can effectively figure out the nuances of educating, influencing, signing up, and serving multicultural customers are poised to accelerate their growth and win significant share.
Carlos Santiago will delve further into this topic during his presentation, The State of Multicultural ACA Marketing: Hurdles, Opportunities & Return, at the MCH National Conference. His presentation examines the relationship between Hispanic dedicated efforts and overall revenue acceleration, the so called ACA feasible/eligible opportunity gap for Open Enrollment 3 and beyond, as well as the Multicultural opportunity coming from this next Open Enrollment. Learn from Carlos, as well as the rest of our esteemed speaking faculty, at the 2015 MCH National Conference, held Oct 12-13 at The Westin in Fort Lauderdale. Register today!


 Taking an inclusive stance toward LGBT consumers can influence non-LGBTs, especially Millennials. Most of us are aware of the fact that Millennials are the most diverse consumer segment we’ve ever seen. And Millennial culture includes respect for and appreciation of diversity, including LGBT. According to Pew, 70% of Millennials support LGBT marriage equality – the highest of any generation. Brands today are taking note of this cultural value and using it as a way to gain sales and share among Millennials. This works particularly well for established brands that are trying to shed an image of being “dated” or not relevant to today’s consumer. Two brands using this approach are Coca Cola, who ran an ad during the Olympics that was a celebration of diversity, including LGBT, and Honey Maid’s This is Wholesome campaign featuring tattooed, interracial, and gay parents in their modern take on the American family. Healthcare could benefit from this more modern image, courtesy of a supportive take on LGBTs.
Taking an inclusive stance toward LGBT consumers can influence non-LGBTs, especially Millennials. Most of us are aware of the fact that Millennials are the most diverse consumer segment we’ve ever seen. And Millennial culture includes respect for and appreciation of diversity, including LGBT. According to Pew, 70% of Millennials support LGBT marriage equality – the highest of any generation. Brands today are taking note of this cultural value and using it as a way to gain sales and share among Millennials. This works particularly well for established brands that are trying to shed an image of being “dated” or not relevant to today’s consumer. Two brands using this approach are Coca Cola, who ran an ad during the Olympics that was a celebration of diversity, including LGBT, and Honey Maid’s This is Wholesome campaign featuring tattooed, interracial, and gay parents in their modern take on the American family. Healthcare could benefit from this more modern image, courtesy of a supportive take on LGBTs.
 Narrow Impact: Fee-for-Value
Narrow Impact: Fee-for-Value Broad Impact: Patient & Lifestyle Autonomy
Broad Impact: Patient & Lifestyle Autonomy