Hypertargeting brings pharma marketers closer to the defined patient populations we all want to reach at the moments that matter for consumers and patients. It’s making it easier for us to address health interests, concerns, and questions with specific guidance and timely insights. We can speak to patients at actionable decision points rather than spending money on awareness campaigns and casting a wide net in an ever-growing sea of marketing messages. Ultimately, the spread of hypertargeting will build higher quality connections and lead to superior patient outcomes.
All of this is good news. But hypertargeting is more than just a messaging or delivery strategy. To make the most of the new techniques that hypertargeting enables, and ultimately invest marketing dollars where they will provide the most benefit, make sure you understand these five things about the new discipline.
Hypertargeting helps you educate
We all understand that in today’s data-driven market, there’s little reason and even less reward to simply blast a brand message far and wide in the hopes of catching a few good candidates. Hypertargeting makes it easier to refine your message and your reach so that more of the recipients are actively looking for answers. It dilutes a brand’s image and trustworthiness when it spends so much time and energy reaching people when they are uninterested and unmotivated, or otherwise consider the message irrelevant to their needs.
Now that hypertargeting can communicate more directly with the people most likely to benefit from a specific medication, it’s time to rethink the way messages are structured. Instead of awareness, brands can embrace the opportunity to start a one-to-one conversation at a deep level in a way that feels serendipitous to the patient. We’re just in the beginning stages of seeing how these new educational messages can be structured, and it’s an exciting time for strategists to experiment.
Hypertargeting unlocks the right locations
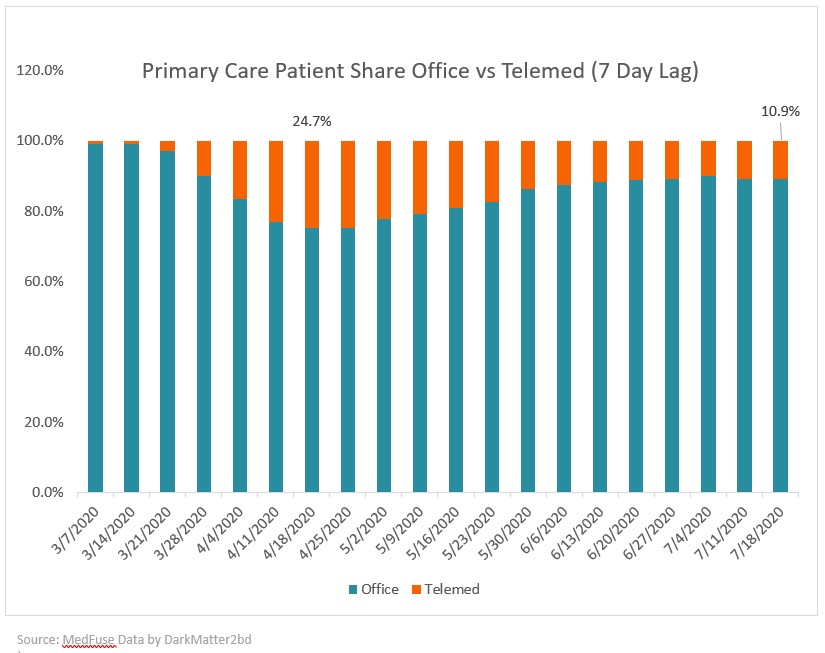
Hypertargeting’s strengths are best realized when we can reach patients in a timely manner. That includes delivering messages that reflect an understanding of where patients (and prospective patients) are on their individual treatment continuum. But it also means opening up to the idea of meeting patients in different ways and in all the locations where care decisions will be timely and relevant to their interests. This includes doctor’s offices and pharmacies, the most common places people seek remedies and pursue treatment. And as a result of the COVID pandemic, telemedicine has become an increasingly relevant touchpoint option in the care path. A hypertargeting strategy that focuses narrowly on a single channel could be just as limiting as one which relies too much on wide-net broadcast.
Hypertargeting needs credibility and transparency
The importance of industry standards for sensible, respectful practices and measurable, auditable processes will only be amplified by hypertargeting. As we gain greater ability to reach patients in new locations and with extraordinarily focused and relevant messaging, we will all collectively have to take responsibility for reaching patients with messages that do not feel invasive and are tonally matched to the environment they’re in.
And with the emergence of new targeting strategies, the need for transparent, verifiable deliveries and results will also grow. Industry players should hold each other accountable to timely deliveries of credible data, and ideally involve a third-party analyst in the validation of performance and results.
Hypertargeting requires robust data and robust strategy
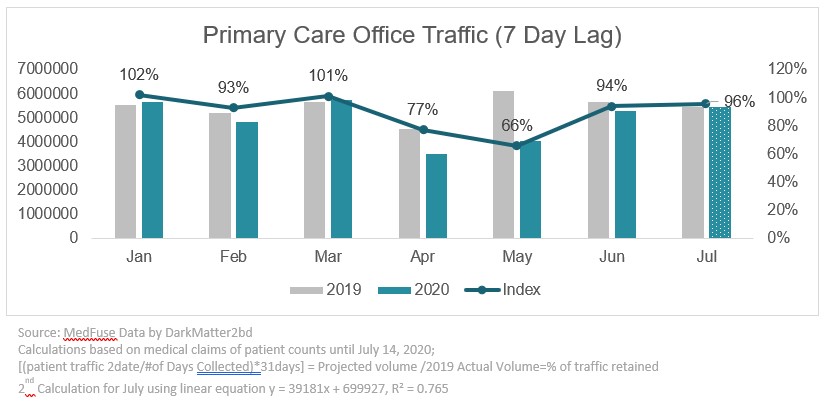
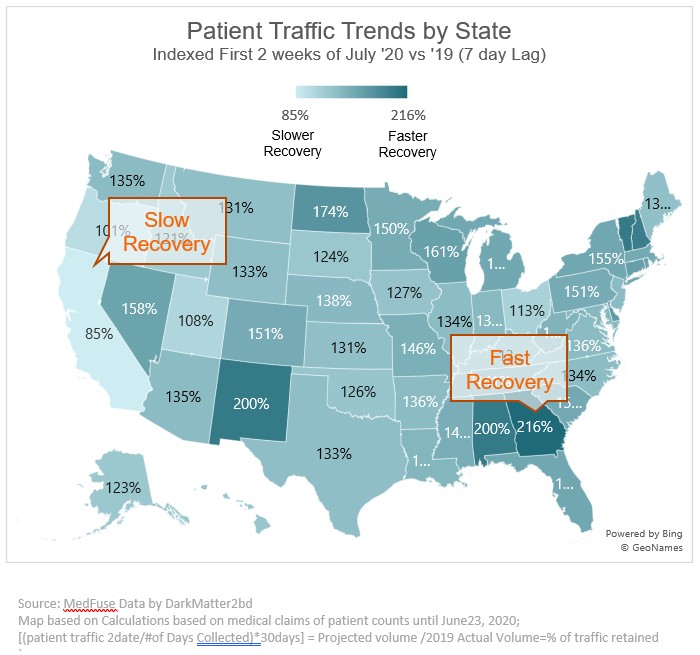
To properly execute a hypertargeting strategy, pharma marketers need more data than ever before. This can include taking deeper dives into sources like retail pharmacy data and demographic insights. To optimize both physical and digital deliveries through hypertargeting, go deeper into connecting data sources including medical claims and Rx claims when possible. These data sources can help identify audiences with the greatest likely need for specific treatments and incrementally improve the focus of your hypertargeting campaigns.
Marketing strategists will also need to think about new ways to act on these deeper data pools, including integrating insights when allowed to reach potential patients at a moment of heightened need or awareness. The most coherent targeting strategy of tomorrow will be based on relationships in the data that marketers haven’t been able or motivated to discover in the past.
Hypertargeting should be measured and held accountable for results
When new strategies come to the fore, it can be tempting to rush to implementation and focus on details like tangible performance metrics later. Pharma marketers interested in hypertargeting should hold this complex strategy just as accountable to rigorous measurement and tangible impact as any other campaign or strategy. And if you are not already moving past soft impact measures like site visits or brand engagement, hypertargeting offers a new opportunity to dig for more.
Tie hypertargeted messages directly to measurement of changes in patient care and outcomes. Just as hypertargeting allows us to be more specific about our intentions and communications, it should be seen as opening a door to more specific understanding of success as seen through treatment and adherence.
________________________________
Soon enough, we’ll be able to drop the “hyper-” prefix and simply see hypertargeting as the natural evolution of communication strategies that have gone from broad to narrow at an accelerating pace. And like so many of our shared priorities in pharma marketing, hypertargeting is just another way to keep the individual at the center of everything we do.